
A neurologist and neurosurgeon explain the surgical procedure in the brain and discuss commonly asked questions.
For some people with movement disorders, such as Parkinson’s disease, essential tremor and dystonia, medications alone are not always enough to control their symptoms.
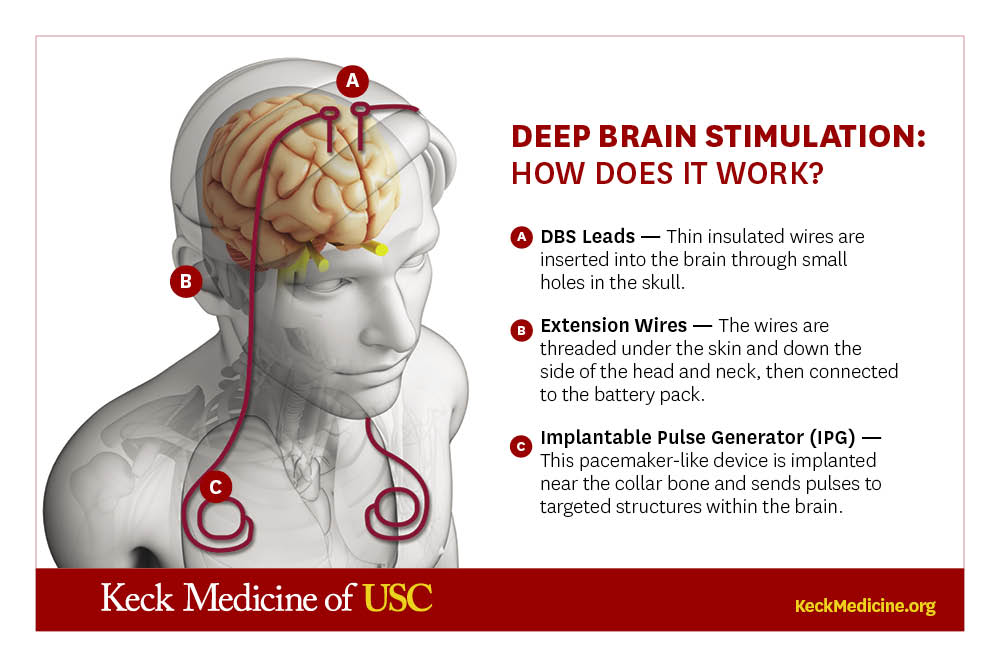
Deep brain stimulation (DBS) — a surgical procedure that involves implanting electrodes into areas of the brain that connect to a device in the upper chest — has proven to be a successful alternative.
The intervention acts like a pacemaker, blocking abnormal electrical signals in the patient’s brain that can cause uncontrolled movements.
“As a neurologist, you often treat patients for conditions in which there is no known cure,” says Xenos Mason, MD, a neurologist at Keck Medicine of USC, who has performed DBS for more than 20 years. “DBS is sort of a miracle in so many ways. You can see the effects of treatment instantaneously.”
He and Keck Medicine neurosurgeon Brian Lee, MD, PhD, answered common questions about DBS.
Who can get deep brain stimulation?
About 20% of patients with movement disorders may qualify for DBS, Dr. Mason says.
Neurologists will evaluate whether DBS would be beneficial for patients who have run the gambit of available pharmacologic therapies and other options, and if their particular symptoms might respond well to DBS.
“As diseases like Parkinson’s progress, medications may start losing their effectiveness,” Dr. Lee says. “Patients start taking higher doses, which can result in side effects. This is where we begin to consider DBS.”
Still, not every candidate is a suitable match.
“Many people with Parkinson’s disease experience freezing of gait, where they suddenly struggle to move,” Dr. Mason says. “This symptom often doesn’t respond to medications or surgery, so that’s not a good match for DBS.
“However, a patient who is struggling to live their daily lives due to a tremor — that’s a symptom that is very well treated by deep brain stimulation.”
What happens during deep brain stimulation surgery?
Deep brain stimulation requires two surgeries. During the first procedure, a neurosurgeon inserts electrodes into the patient’s brain.
Traditionally, patients remain awake for this surgery. “But we can also do the entire surgery inside the MRI scanner with the patient asleep,” Dr. Lee says, noting that the USC Deep Brain Stimulation Center at Keck Medicine is the only DBS center in Southern California that offers this technique, and that both approaches are equally safe and effective.
Patients recover in the hospital for several days before returning in about two weeks for the second surgery, which involves placing a battery device called an implantable pulse generator (IPG) in the chest.
Then, a neurosurgeon connects that device to the electrodes in the brain via wires that run under the skin down the patient’s neck.
“Patients may feel two ‘bumps’ on the top of their head where the wires go into their brain,” Dr. Lee says. Recipients may feel the cable in their neck and be aware of the 2- to 3-inch device in their chest, he adds, but most people adapt quickly and don’t feel any discomfort or pain.
Dr. Lee says the risk of a serious brain bleed during DBS surgery is less than 1% and that the risk of infection is rare (about 3% to 5% of cases) and can often be treated with antibiotics.
How does a DBS device work?
After a few weeks, a neurologist activates the DBS device for the first time.
“The electrodes we placed in the brain have multiple contact points that can deliver electricity,” Dr. Mason says. “We can adjust the spot where electricity is released, the intensity of each pulse and the number of times per second that stimulation is given.”
Results can happen immediately. “Somebody can walk out of your office feeling so much better than when they walked in,” Dr. Mason says.
Patients should expect regular appointments with their neurologist for 3 to 6 months to determine the setting that will provide the most relief from their symptoms. The DBS device is programmed using an encrypted wireless transmitter, so doctors can conduct follow-up visits with patients via video chat and make adjustments remotely.
The chest implant requires a battery replacement every 3 to 5 years. “We do have a rechargeable version that can last 15 years, but that device needs to be recharged regularly to prevent it from running out of electricity,” Dr. Lee says.
What is the quality of life for people with a DBS device?
Once turned on, the DBS device operates continuously — sending electrical pulses at programmed settings — to control a patient’s symptoms.
“Deep brain stimulation doesn’t prevent the patient’s disease from progressing, and it’s not a cure,” Dr. Lee says, noting the device can still offer a long-term solution. “However, DBS can significantly improve a patient’s quality of life, and it allows them to reduce their medications and associated side effects.
“There are no physical limitations; patients can do any activities they could before DBS surgery.”
DBS is currently being explored as an option to treat depression, anxiety and Alzheimer’s disease, Dr. Lee says. The treatment may also help patients with conditions such as obsessive-compulsive disorder and epilepsy.
Topics
