A cardiac electrophysiologist’s opinion on using pulsed field ablation in practice.
FDA’s approval of two pulsed field ablation (PFA) systems for treatment of atrial fibrillation in the past year set the cardiology field abuzz. PFA is now part of the treatment toolbox for certain types of atrial fibrillation.
Not many clinics offer PFA treatment yet, but Ivan C. Ho, MD, director of cardiac electrophysiology at the USC Cardiac and Vascular Institute, part of Keck Medicine of USC, discussed his own experience thus far using PFA for catheter ablation in patients with atrial fibrillation.
Radiofrequency ablation and cryoablation
The most common catheter ablation procedures for atrial fibrillation today are radiofrequency ablation (used approximately 75%-80% of the time), followed by cryoablation (used about 25% of the time), says Ho. Both techniques eradicate arrhythmogenic tissue causing abnormal cell conduction and heart rhythm.
One drawback to radiofrequency ablation and cryoablation is that while both techniques cauterize arrhythmogenic tissue, they run a small risk of damaging adjacent tissue in the process. “We’ve had increasing control on where we destroy the arrhythmogenic tissue over the years with refinement of these techniques, but the thermal nature of both energy sources means that collateral damage to neighboring structures is sometimes unavoidable,” Ho says.
Take radiofrequency ablation. Radiofrequency ablation concentrates radiofrequency energy in the small tip of a catheter where it is converted into heat energy. “By and large, it’s a very controlled procedure, but like anything else, radiofrequency energy is not perfect,” says Ho.

For instance, one of the most common areas of the heart to ablate is the left atrium, near the esophagus. When the catheter tip is applied, “Radiofrequency ablation can generate heat in the neighboring tissue — and the esophagus should not be heated up,” Ho says. “The complications of doing so could be serious, including causing a fistula to form. Thankfully, that’s rare, as it can be a very serious complication.”
Radiofrequency ablation could likewise endanger the phrenic nerve, he says. “Some people get diaphragmatic paralysis as a result, which is a very unpleasant complication.”
Meanwhile, cryoablation takes a similar approach to destroying tissue but by using extreme cold rather than heat. It, too, can risk causing collateral damage. “Instead of thermal injury of neighboring organs by heat, it’s thermal injury by cold,” Ho explains.
Yet despite these risks in a small percentage of cases, both cryoablation — and radiofrequency ablation especially — are still considered safe overall and widely used in practice, Ho says.
Pulsed field ablation is the next generation
PFA emerged as a next-generation concept for catheter ablation for atrial fibrillation over a decade ago, but it took a good part of the last 10 years to perfect and test this new energy source in order to ensure it is safer and as effective — if not more so — than radiofrequency energy.
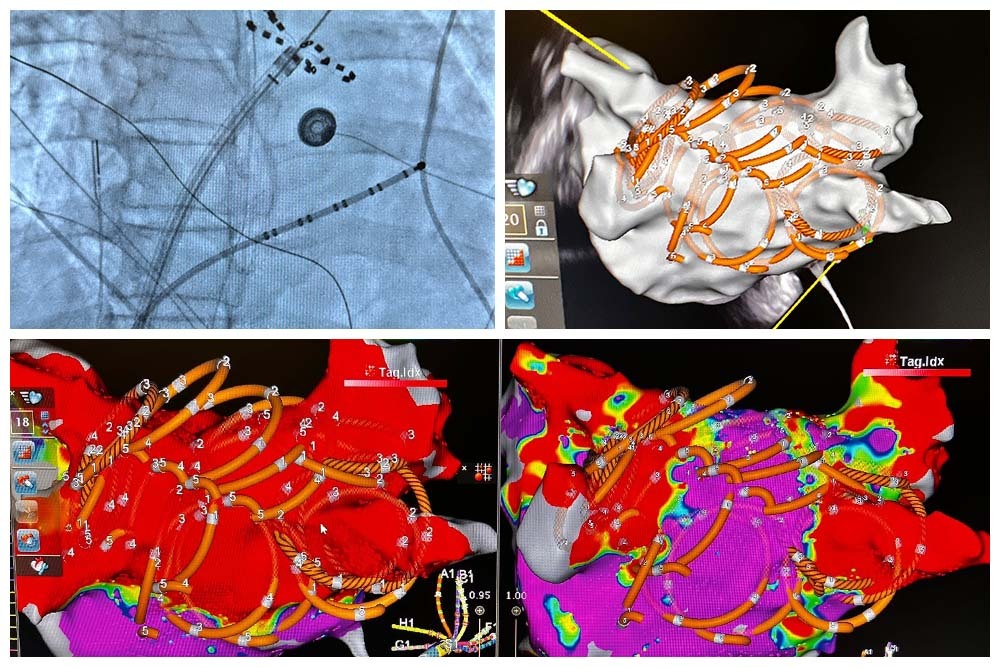
PFA uses irreversible electroporation to deliver high-voltage, short-duration electrical pulses that irreversibly damage the cells of diseased tissue.
“It’s basically punching holes in these electrically active cells of the heart,” Ho explains. “These highly tuned waveforms carrying high-voltage pulses create holes in the cell membrane, disrupting the membrane’s phospholipid bilayer structure and rendering these cells no longer electrically active. It does this without any thermal effect on neighboring structures.”
“This,” he says, “is ideal energy, because it affects the tissue we want to get rid of, and it doesn’t cause collateral damage.”
For some atrial fibrillation patients, PFA could be a safer alternative to radiofrequency ablation and cryoablation.
Health care systems may also see some practical benefits from using PFA. “From the hospital perspective, it’s a much quicker procedure,” Ho explains. “With PFA, each pulse takes only about four seconds each, whereas with radiofrequency ablation, each burn can take between 20 and 40 seconds to achieve. This means that with PFA, the duration of a procedure can be reduced from more than two hours to about one hour. It’s faster, safer and just as efficacious. That’s why it’s such a big deal.”
Knowing when to use PFA in practice
It takes an expert to know when a patient is a good fit for PFA. Fortunately, PFA could expand the number of atrial fibrillation patients who can undergo ablation, says Ho.
“For sicker, older patients especially, PFA is a good option because radiofrequency ablation is a longer procedure requiring general anesthesia. We also need to use more IV fluid during radiofrequency ablation. Older, sicker patients with cardiac issues may not tolerate these conditions well. Sometimes, we won’t even do ablation on these patients for this reason. Because PFA is shorter, easier and safer, we can extend ablation to patients we otherwise normally would have had to think very hard about ablating before.”
What to watch for
Despite its promise, Ho cautions that PFA has not been studied for as long as radiofrequency ablation and cryoablation.
“Radiofrequency ablation still has the longest track record because it’s been used for almost 40 years,” says Ho. “These studies have shown that radiofrequency ablation is safe, and we know what’s good about it and we know what’s risky about it.”
By contrast, he continues, “PFA has only been in clinical use for about five years at most. We don’t know what happens to patients 15 years later. We don’t have that information. If you are conservative and not an early adopter, you might wait to try PFA.”
Also, he adds, “The data published on PFA is mostly for paroxysmal atrial fibrillation, the earliest stage of Afib.” Cardiology experts are still discussing the efficacy of PFA for persistent Afib. “There’s no clear strategy agreement on persistent Afib,” Ho says.
Moving forward with PFA
PFA will undoubtedly be a prominent topic in the cardiology field for years to come.
“I feel like people just need to know that this is an exciting technology that we think has a very promising future. We can’t say that it is as good as radiofrequency ablation yet because it doesn’t have as much data behind it, but the early signs are extremely good,” Ho says. “It was good enough for FDA to approve it ahead of schedule, and they rarely do that.”
The USC Cardiac and Vascular Institute began offering PFA treatment this May, and some patients are expressing interest in the option. But, Ho says, he and his colleagues will ultimately use their expertise to judge who would be a good candidate. “We tend to be quite thoughtful because a lot of sicker patients needing ‘redo’ treatments are sent to us, so we would do more strategizing about whether or not to use PFA,” he says.
Radiofrequency ablation won’t be phased out either, he says. “I think we’ll use PFA on a case-by-case basis, but I don’t think it will ever replace radiofrequency ablation. Radiofrequency ablation is just so reliable. It’s an established and mature technology. Also, PFA as of now has only been tested for certain types of Afib, so for other types of Afib, we’ll go back to using conventional methods like radiofrequency ablation.”
“But,” he says, “I think pulsed field ablation will eventually take a dent out of the radiofrequency ablation market.”
Topics
